View more featured posts
More insights and updates from Mindstate Psychology.
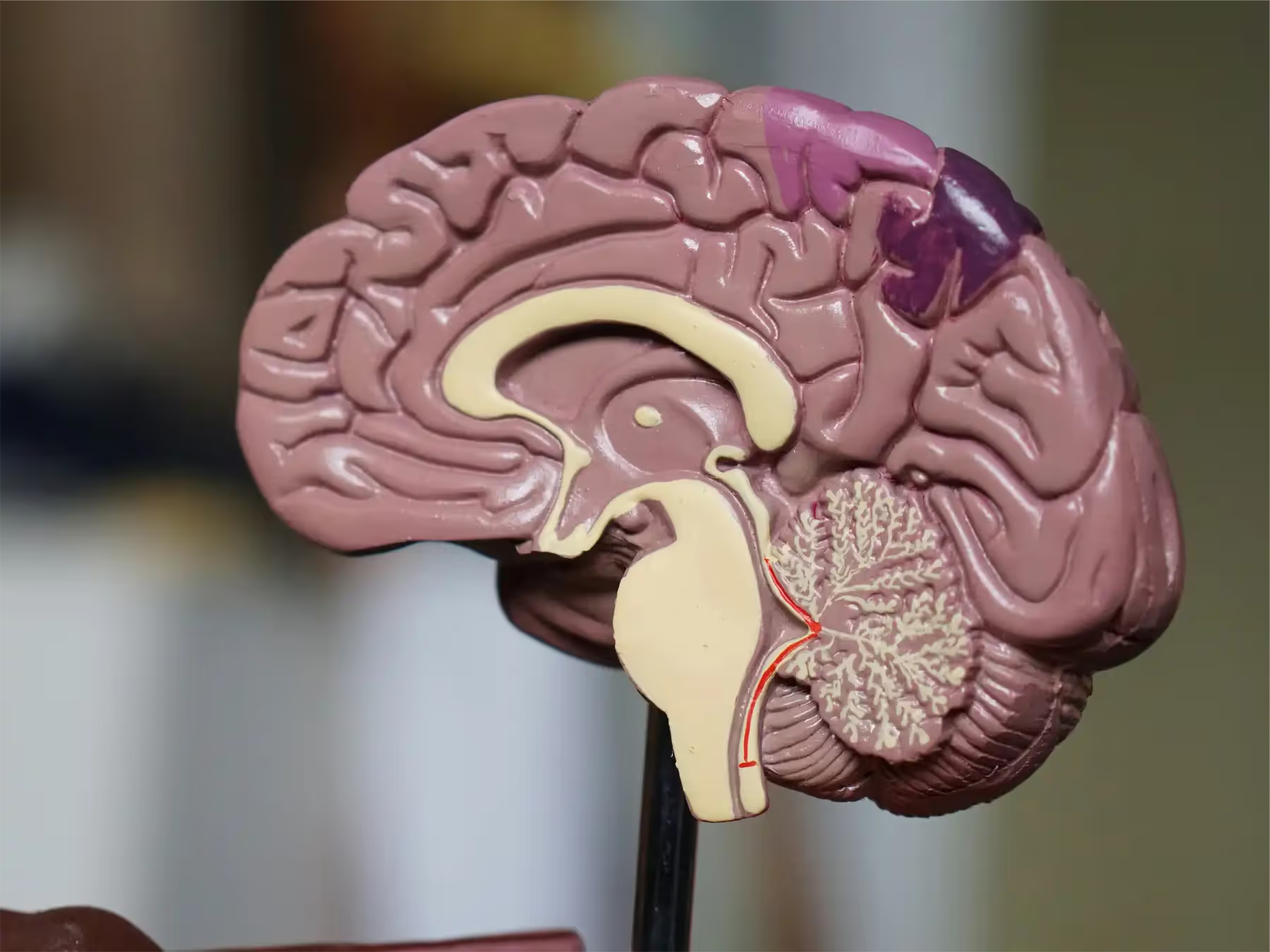
Alzheimer’s Disease (AD) research is undergoing a transformative shift. No longer limited to symptom tracking and broad disease staging, the field has increasingly embraced a biomarker-driven approach that promises earlier detection, more accurate prognosis, and individualized intervention strategies. In particular, neurophysiological biomarkers now offer critical insights into the underlying mechanisms of cognitive and functional decline in Alzheimer’s.
The pursuit of reliable biomarkers for AD has led to the identification of a wide range of biological indicators across various domains:
While each biomarker type contributes valuable information independently, their true power lies in integration. Multi-modal approaches—linking genetic, fluid, and imaging data—reveal complex interactions that better explain individual differences in symptom presentation and treatment response.
Recent studies have begun to delineate how specific biomarkers relate to distinct functional and cognitive impairments:
This mapping not only supports earlier and more accurate diagnosis but also informs personalized treatment planning, enabling clinicians to tailor cognitive rehabilitation strategies or lifestyle modifications to the patient’s unique biomarker profile.
Perhaps one of the most exciting frontiers in AD research is the study of neuroelectrical and physiological responses—particularly how they are modulated by non-pharmacological interventions such as physical activity, cognitive training, and neurofeedback.
Emerging evidence suggests that interventions like aerobic exercise and mind-body practices (e.g., Tai Chi, yoga) not only improve cognition but also induce measurable changes in brain oscillatory activity, such as enhanced alpha and theta power. These changes may reflect improved synaptic plasticity and functional connectivity.
Excitingly, research is in the early stages of examining the role of EEG neurofeedback as a potential treatment to address address cognitive deficits and behavioral changes in dementia and other neurological disorders. The study found that EEG Neurofeedback was effective in improving at least one cognitive domain.
Despite these advances, many mechanistic questions remain. We still lack a complete understanding of:
Additionally, much more research is required to examine the potential role that Neurofeedback could play as a potential treatment for Alzheimer's. As research advances, integrating EEG neurofeedback into Alzheimer's treatment may pave the way for more personalized and effective therapeutic regimens. It's certainly an area we watch with great interest over the coming years.
Interested in what neurofeedback at Mindstate Psychology can do for you today? You can discover more about the conditions we use neurofeedback to help here, or contact us to arrange a free telephone consultation.